Career Ladder Bias: “How To Succeed” Inside The Medical-Industrial Complex.
Posted on | November 15, 2017 | 2 Comments

Mike Magee
In 2004, when I read Dr. Marcia Angell’s book, “The Truth About the Drug Companies: How They Deceive Us And What To Do About It”, I agreed with everything she wrote. How couldn’t I? At the time, I had a front row seat inside the largest pharmaceutical company in the world and managed a substantial external-facing portfolio that included “Medical Relations.”
But what was equally obvious to me was a glaring omission. Dr. Angell had largely let academic physicians and their institutions and associations off the hook. My “front row seat” not only revealed the underbelly of Pharma coercion, but also how willing were many of the top physician leaders in both academic and organized medicine to participate.
If this was a secret, it was hiding in plain sight. In 1966, Henry Beecher couldn’t have been clearer when he wrote in Dr. Angell’s New England Journal of Medicine, “Every young man knows that he will never be promoted to a tenure post, to a professorship in a major medical school, unless he has proved himself as an investigator. If the ready availability of money for conducting research is added to this fact, one can see how great the pressures are on ambitious young physicians.”
What I knew to be true then, and what is even truer now in our modern entrepreneurial gold rush built around genomics and stem cells and personalized therapies, is that the Medical-Industrial Complex’s strangle hold on our inefficient and often ineffective health delivery system is based on an integrated career ladder that moves from academia to industry to government and back again.
As Dr. Beecher correctly noted, publications and presentations are both the admission ticket to the ground floor of medical academic success, and the escalator to a higher perch in a gilded cage brimming with direct and indirect rewards.
To sustain such a system requires a wide range of collaborators and benefactors. To succeed, one must, at times, turn a blind eye. One does not “go along” unless one “gets along”. Publications are followed by several rounds of amplification, first at CME meetings and association panels, then through NIH grants and inclusion in government or industry advisory boards, and finally with an invitation for membership within national associations, foundations and governmental science boards.
That our medical science system is chronically rigged has led to a number of charges of late. Most have involved NIH funding where the claim is that grants are over-weighted toward well-known investigators and blue-chip institutions. For example 40% of the dollars are awarded to 10% of the grantee institutions.
But what about bias in the selection for publication or for a slot at the podium of a prestigious meeting? An October 10, 2017 article in the Proceedings of the National Academy of Sciences sheds some light on these questions. The authors are luminaries in the computer science field and were asked to jury submissions for the 10th International Machinery Conference on Web Search and Data Mining (WSDM 2017). In the academic computer science world, “research typically appears first and often exclusively in conferences rather than in journals.” And WSDM 2017 is one of the largest meetings.
Historically, only 15% of submissions to the WSDM are chosen. The process involves a large group of expert reviewers who each read and grade four submissions using a system that allows them to enter “bids” which are necessary to be in the running at all for a spot. Reviewers then grade the submitted bids. Those entered and possessing the highest marks prevail.
The WSDM has always used a single-blind reviewing process. This means that the reviewers know the names and affiliations of those submitting a proposal, but the potential presenter never knows the name or affiliation of his or her reviewer. JAMA employs a single-blind review process in peer-reviewing their journal submissions. At the time the authors were beginning their WSDM 2017 deliberations, the question was raised whether the organization should move to a double-blind review. In this method authors and reviewers and their affiliates are anonymous to each other. That is reviewers must judge purely on the merits of the submission without considering the source.
The authors, Andrew Tomkins and Min Zhang, elected to design a study using the 2017 process to inform recommendations for the 2018 conference. They created two parallel reviewing processes and split reviewers. 974 were double-blind and 983 were single blind. In analyzing the results, they detected statistically significant bias as follows:
- Single-blind reviewers who knew authors and their institutions voluntarily restricted bids. That is, they held back bidding keeping larger numbers from competing for spots on the program. In all they had 22% fewer entry bids than did their blinded counter-part reviewers.
- Single-blind reviewers in assessing those fewer bids they had placed in the running, were significantly more likely to recommend famous authors and those from famous institutions for acceptance.
As a result, the authors recommended that WSDM 2018 move to a fully blinded review process.
Tags: Conflict of Interest > International Machinery Conference on Web Search and Data Mining > JAMA > medical-industrial complex > MIC > NEJM > NIH > WSDM
What’s the best specialty for a medical student who wants to be a progressive politician?
Posted on | November 13, 2017 | 2 Comments

Mike Magee
If you are a medical student and aspire to be a progressive political leader as well, what might be the best specialty tract to pursue?
You could chose pediatrics as Ralph Northam did, and receive your training in the military, retiring at age 33 as a major and then become a pediatric neurologist at a Children’s Hospital in Norfolk, Virginia and eventually serve as governor of Virginia.
Or you could be an internist and join one of the public health units of NIH at the age of 28, and find yourself at the center of every politically charged public health crisis ever since like Tony Fauci, NIAID director, did.
You might be a surgeon like Susan Love whose advocacy for women’s health included a campaign against routine estrogen use to treat menopause, and who has been advocating for women ever since while serving on the National Cancer Advisory Board and the National Cancer Institute since 1998.
Or you could chose Family Medicine like Nancy Dickey did, before delivering some 4000 babies, becoming the first female president of the AMA in 1997, and then spending more than a decade as a president of a major university as she did at Texas A&M.
All good…but if you want to be where the action is and have a front row seat to view the impact of policy and leadership gone wrong, Emergency Medicine might be the place to go.
As Neal Flomenbaum, Editor-in-Chief of Emergency Medicine, suggests in this month’s issue, you will certainly gain an education.
Neal catalogues the natural and unnatural disasters that have appeared on Emergency Medicine’s doorsteps in just the past 10 months including:
* 3 Gulf Coast/Atlantic hurricanes and a West Coast fire claiming 285 lives.
* Unnatural shootings and attacks in LasVegas, New York City, and Sutherland Springs, Texas leading to 84 deaths and 558 injuries.
* Nationwide, in just 10 months, 52,719 shooting incidents which left 13,245 dead and 27,111 injured.
Neal quotes the October 9, 2017 Wall Street Journal article by Jeanne Whalen whose title “Training Ground for Military Trauma Experts: U.S. Gun Violence” seems to suggest that doing a stint in a domestic trauma center should be a prerequisite to joining the medical military in Iraq.
There’s little doubt that is you chose this option as a progressive stepping stone, you’ll develop real life skills and gain an unvarished view of what’s wrong. But as Tom Scalea, a trauma surgeon in Baltimore suggests, you’ll need more than that if long-term solutions are your bailiwick.
Tom said, “Mass shooting? That’s every weekend.…it makes me despondent….I don’t have the ability to make that go away. I have the ability to keep as many alive as I can, and we’re pretty good at it.”
Neal is one step ahead of us when he writes, “As for preventing deaths from natural disasters, more accurate weather forecasting and newer technology offer more hope. Among the 134 storm related deaths from Hurricane Irma in September, 14 were heat-related after the storm disabled a transformer supplying power to the air conditioning system of a Hollywood, Florida nursing home.”
So, for you, the medical student, who loves medicine, loves politics, but also loves people more than power, the truth is, there are a number of pathways toward progressive success.
But in making your choice, I’d ask yourself these three questions:
1. Where is my heart leading me right now in the service of others?
2. Am I willing to train and then utilize the skills I have accumulated to not only care and comfort individuals, but also serve and lead our nation in a positive and hopeful direction?
3. As I mature, when I mature, am I confident that my core values will hold? Will I remain strong enough, secure enough, progressive enough to guide our nation and our culture toward durable and permanent solutions? Will I stay true to myself and not succumb to greed, self-loathing and hatred?
If so, if given the chance, I’ll vote for you.
Tags: emergency medicine > health care leadership > medical leadership > nancy dickey > neal flomenbaum > progressive leaders > progressive politics > ralph northam > susan love > Tony Fauci
What Friedman and Sandel and Desmond (and Maine) Know About Our Nation’s Health.
Posted on | November 7, 2017 | 4 Comments
Niger and Waco
Mike Magee
We wake this morning to news that Maine voters have overrode their own governor and expanded ACA Medicaid, and Virginia voters have rejected a Trumpian appeal. As we begin to turn the corner, we need to be certain we don’t simply return to neutral but instead understand and execute progress. Health policy is the ideal catalyst.
When it comes to policy matters (whether they be related to taxes, or guns, or advertising), Canada historically has exhibited great natural instincts and a healthy dose of holistic common sense.
Consider the fact that at the end of WWII, with veterans streaming back into the country weighed down with a heavy burden of diseases, addictions, and psychiatric disabilities, Canadian leaders realized that the success of their country ultimately would depend on the health of Canadians. They wisely saw health as a human right, and realized that lack of coordinate health planning coupled with excessive free marketering would drive up cost and complexity, placing an undue burden on all of their citizens.
Compared to Canada which chose universality and simplicity, following WW II we elected to stay mired to individualism and “free enterprise” approaches reasoning that if we could beat the Nazis, we could easily beat disease, and health would thrive in its wake.
The results of this unending experiment have been singularly disappointing. Scientific progress has become unlinked from human progress. One in five dollars is now committed to a speculative Medical-Industrial Complex that continues to grow in size and appetite. And the gap between have’s and have-nots leaves a gaping hole in our national stability, optimism, and civility.
Our failures in the health sector increasingly draw comparisons to developing nations rather than to our historic developed peer nations. Fundamentally, we seem so infatuated with discovery, patents, and corporatized solutions that we manage to silently deny that health is a function primarily of social determinants.
Tom Friedman understands this. He recently focused on the struggles in Niger which came under a glaring spotlight when we lost four U.S. Special Forces in a battlefield that most Americans didn’t know existed.
Friedman wisely focused not on the losses, as tragic as they were, or even the conflict itself, but on the underlying causes. The destabilization of this region in Africa and the explosion of “economic migrants, interethnic conflicts and extremism” is tied to the ever “widening collapse of small-scale farming”. That collapse, in turn, is a function of four intersecting triggers – climate change, Saharan desertification, population explosion (Niger’s birthrate is 7.6 children per woman), and misgovernance.
In light of the above, how does America’s president respond beyond putting our soldiers at risk? By eliminating U.S. support for global contraceptive programs; by supporting climate deniers; by pushing exportation of coal to Africa; and by curbing climate research.
It would be easy to suggest that Trump is an outlier, but as we hot-tail it to “personalized medicine” and stem cell this and that (all good but speculative and of little impact on immediate population health), we way miss the forest from the public health trees.
For example, Megan Sandel and Matthew Desmond this week laid out the connection between health and housing. But was anyone but John Kasich listening?
A few facts:
1. In America, “2.8 million renting households are at risk of eviction and more than 500 000 people are homeless on any single night.”
2. “Only 1 in 4 households that qualify for housing assistance receives it… most renting households below the federal poverty line spend more than half of their income on housing costs, and 1 in 4 spends more than 70% of its income on rent and utility costs alone.”
3. “Rent-burdened families not only have less money to spend on wellness and health care but also regularly face eviction and homelessness, which further threaten their health.”
4. “Housing problems have been associated with a wide array of health complications, including lead exposure and toxic effects, asthma, and depression.”
5. “The top 5% of hospital users—overwhelmingly poor and housing insecure—are estimated to consume 50% of health care costs.”
6. “Randomized trials have found that hospital stays and emergency department visits decreased among homeless individuals after they were offered stable housing and case management.”
The authors conclusions:
Friedman: “ Nothing Trump ever says has a second paragraph. His whole shtick is just a first paragraph: Build a wall, tear up the Iran deal, tear up TPP, defeat ISIS, send troops to Niger and Afghanistan to kill terrorists, kill climate policy, kill family planning, cut taxes, raise military spending. Every box just marks an applause line he needed somewhere to get elected. Nothing connects — and we will pay for that.”
Sandel and Desmond: “ A stable home functions as a secure foundation on which to build holistic and cost-effective health care. Without this foundation, medical treatments are reduced to short-term, limited fixes that must be applied and reapplied at significant cost and insignificant health gains. Hospitals and health systems can and must do better in investing in homes for health, for both patients and the broader community.”
And Kasich, to a major GOP donor who challenged his support of Medicaid expansion in Ohio at a Koch brothers conference: “I don’t know about you, lady, but when I get to the pearly gates, I’m going to have an answer for what I’ve done for the poor.”
Tags: health and housing > health policy > JAMA > John Kasich > Niger > NYT > public heal > Social determinants of health > Thomas Friedman
Disrupter in Chief – CVS, Aetna, or Amazon?
Posted on | October 30, 2017 | 3 Comments

Mike Magee
In 1964, a purveyor of general merchandise based in Rhode Island, coalesced 17 locations under one entity. They were focused on market data, inventory management, and economy of scale. Within five years, they were successful enough to have 40 locations, three with in-store pharmacies.
Within another decade, they had standardized their information, data, and business systems, and their annual sales had long exceeded $100 million. By 1985, they topped $1 billion. They now have 9,700 stores and in 2016 generated over $200 billion in revenue with 60% coming from pharmacy services. Their original name was Consumer Value Stores, but now everyone just calls them CVS, the seventh biggest corporation by revenue in the United States.
You might say they were the original disrupters in health care. And they’ve tried to keep their eye on the ball. For example, they’ve known that internet sales were a threat to their retail non-drug sales. Three years ago, in-store general purchases made up 52% of their revenue. Now it’s only 46% and continues to drift south. In response, they’ve looked at the lucrative U.S. pharmaceutical 4.5 billion prescriptions per year market worth $560 billion a year for every conceivable angle.
Some years back, CVS tip-toed into the provider space with their in-store Minute Clinics. That’s been a partial success. In 2007, they purchased Caremark, a pharmacy benefit manager, to capture supply chain management revenue, and that’s been good. They signed up insurer Aetna to a 12-year PBM contract in 2010. They’ve thought about more horizontal expansion – more stores – but the federal government rejected a bid by their arch rival Walgreen when it attempted to merge with Rite-Aid drugs, viewing it through an anti-trust lens. The feds did the same thing in blocking two different attempts by health insurers to merge last year.
For CVS, it’s been difficult to sit still and watch others go vertical. Take UnitedHealth Group, the insurance giant started by a physician, which now also owns its own PBM under the health services banner, Optum. They’re doing great with 3rd quarter earnings up 26%. Then there’s Anthem, the BC/BS insurer, that got in a nasty fight with their former ally, stand-alone PBM, ExpressScripts. Now Anthem is also starting its’ own PBM. Together Caremark, Optum and ExpressScripts control 80% of the PBM market.
Four months ago, health analyst Robert Flynn pointed CVS in the vertical integration direction, providing six reasons why he thought they ought to buy insurer Aetna with access to their 22 million customers. The reasons included that horizontal merger consolidation options were no longer feasible; competitors like United-OptumRx were gaining traction; the risk would be low since Aetna was already a Caremark customer; it would beat Express Scripts to the punch either as an insurance purchaser themselves or alternately being purchased by Walgreens; and the vertically oriented CVS-Caremark-Aetna goliath would be in a good position to do value-based contracts – like those advanced for Hepatitis-C cures.
So with this kind of forecasting, it shouldn’t have been big news last week when CVS and Aetna announced that negotiations for a CVS $66 billion buy-out of Aetna was underway. Their combined valuation would exceed $240 billion. But strangely enough, the original health disrupter in chief was out-disrupted by the ultimate disrupter of all, Amazon.
The New York Times headline said it all – “CVS and Aetna Talks Take Place Under Amazon’s Shadow.” What triggered this take-down was a new report in the St. Louis Post-Dispatch a day earlier that Amazon had won approval for wholesale pharmacy licenses in 12 states (NV,AZ,ND,LA,AL,NJ,MI,CT,ID,NH,OR,TN).
 “There are a lot of differences between books and drugstores, but there are a lot of similarities, too. Customers want selection, convenience, price and information.” Jeff Bezos, Amazon CEO
“There are a lot of differences between books and drugstores, but there are a lot of similarities, too. Customers want selection, convenience, price and information.” Jeff Bezos, Amazon CEO
The stories trumpeted Amazon’s market cap of $524 billion, and their history of upending other sectors like cloud computing, logistics and groceries. Marketing professors like Scott Galloway of NYU turned to florid prose. His prediction: “You will see strange bedfellows. P&G and Unilever, Nike and Adidas are going to come to the realization that they are competitors, not enemies. Their real enemy is in Seattle. When German tanks rolled into Slovakia and Poland, the Russians, British and Americans found a way to get along. The tanks {Amazon} have rolled in.”
CVS CEO Larry Merlo didn’t seem phased. He said, “We’ve seen threats in the past, OK.” He’s presuming that health care is different, too complicated for Amazon. But complexity is the pay-dirt that could bring success out of failure. Consider this model transaction as it exists today:
Original Stream:
Step 1: Pharma Company sets a price of $100 as the list price for 30 day supply of XYZ pill.
Step 2: Pharma Company marks-up the wholesale price to $110 and sells to one of three giant national wholesalers (McKesson, Cardinal, AmerisourceBergen).
Step 3. Wholesaler bumps price to $120 and sells to pharmacies.
Step 4. Pharmacy marks the price up to $130.
Secondary Back-Stream:
Step 5. Insurer Pays PBM $140 but receives a $45 rebate from the PBM. (Net payment by insurer is $95.)
Step 6. That $45 payment to the insurer came from a $50 rebate from the Pharma company. PBM keeps $5 of the rebate for itself. (Pharma profit: $110 -$50 = $60)
Step 7. PBM pays $110 and patient co-pays $20 to the pharmacy. (Pharmacy keeps $10.)
Step 8. PBM nets $35 profit. (Difference between $140 from insurer, and sale to pharmacy/patient for $110, plus $5 from Pharma’s $50 rebate)
You think Amazon might be able to figure out how to skip a few of these steps – like the wholesaler and the retailer and the PBM? And that doesn’t even consider the possibility that Seattle and Washington, D.C. might discover each other along the way.
Tags: amazon > Caremark > cvs > CVS Aetna merger > drug costs > drug rebates > Express Scripts > Optum > UnitedHealth
Single Payer Health Reform – A Solution For U.S. Income Inequality?
Posted on | October 26, 2017 | Comments Off on Single Payer Health Reform – A Solution For U.S. Income Inequality?
Mike Magee
Veteran Health Policy expert, James A. Morone, Ph.D., makes an interesting argument for single payer health care in this week’s NEJM. In proposing a sweeping change that would directly address “the American patchwork”, assert “the norms of communal decency”, promote planning and efficiency, and empower “a righteous band of reformers, deeply committed to a cause, pushing against all odds”, he does not sidestep higher taxes on the rich.
Rather he sells into them, presenting high taxes on the rich in return for universal health coverage as “on a short list of available policies designed to push back on inequality.
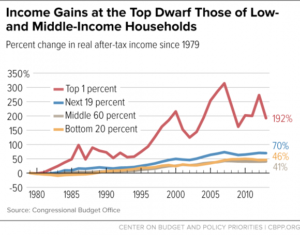
His argument boils down to the fact that a certral element of the national crisis we call “Trump” is populist anger grounded in remarkable income inequality. In roughly a half-century, our separation between rich and poor which used to mirror France and Japan, now aligns with Mexico and Brazil.
In short, we’re a mess, and our citizens are pretty fed up. And why shouldn’t they be? Our top 1% controls roughly 40% of all wealth, while the bottom 90% manages a paltry 23%. If you’re a white family in America, you were born lucky. On avaerage, your family is about 10 times as wealthy as your black family counterpart.
But what about taxes, and distrust of “Big Government”? Morone reminds us that major policy changes can, and have, flipped on a dime in the past. As he says, “Disruptive populism ended past American gilded ages, and it shows signs of challenging the current one.” With better health delivery, and more equality and social justice, we might also redirect the course of American politics and American politicians.
In the same issue of NEJM this week, Henry J. Aaron, Ph.D., explores different roads to reform, raising legitimate concerns about the unintended consequences of disrupting existing insurance holders, and arguing for a more cautious incremental approach including extending availability of Medicare and Medicaid to others, and shoring up ACA exchanges. He wonders how far and how fast are Americans willing to go?
This week, New York Times columnist, Thomas Friedman, shared his view. He didn’t pull punches when he accused Trump of intentionally undermining the two critical pillars of American society, truth and trust.
Interestingly, in the careful analysis of these two health policy experts above, both identify an embattled and epic American struggle over how to topple the health care status-quo, a Medical-Industrial Complex controlled and directed by members of the 1%, and a debate that currently hangs on whether we – the citizens – are able to discern fact from fiction.
The key question for health reform and for the future of America: Do we trust a government “of, by, and for the people” to assure that each of its citizens has the right to “life, liberty, and the pursuit of happiness?”
If a majority of us can move to “yes” on that question, we will find a way to embrace each other equally through health reform. And the quality and durability of that embrace will be determined by these Code Blue principles:
1. Universality: Health coverage is a right of citizenship.
2. Public Administration: Administration of basic health coverage is organized in the most cost-efficient manner possible with central oversight by the government.
3. Local Control of Delivery: The actual delivery of services is provided by health professionals and hospitals at the local and state levels.
4. Health Planning is a Priority: Creating healthy populations is a high priority on the federal and state levels.
5. Transparency: Providers submit bills. Government ensures payment of bills. Patients focus on wellness or recovery.
Tags: health care a right > health care reform > Henry J. Aaron > James A. Morone > NEJM > single payer > Thomas Friedman > universal health care
Why are cigarette smokers congregating in Unhealthy States?
Posted on | October 23, 2017 | Comments Off on Why are cigarette smokers congregating in Unhealthy States?

Will Rogers on Fellow Okie, Scott Pruitt.
Posted on | October 17, 2017 | Comments Off on Will Rogers on Fellow Okie, Scott Pruitt.

Mike Magee
Oklahoma’s favorite son, Will Rogers, once said, “Live in such a way that you would not be ashamed to sell your parrot to the town gossip.”
On August 2, 2017, that parrot was doing overtime, and he kept squawking, “Pruitt, Pruitt, Pruitt.” That’s because Oklahoma had just experienced 7 earthquakes in 28 hours. Scientists agree that these increasingly common geological events, rare in the state until 2009, are the result of injecting heavily contaminated fracking wastewater in underground disposal wells.
Adding insult to injury is President Trump’s appointment of former Okie attorney general, Scott Pruitt, as head of our nation’s Environmental Protection Agency. That’s the very same agency to which he had mailed a letter requesting regulatory relief using exact oil company text cut and pasted onto his official state stationary. That little offense was after he had challenged core results of climate scientists on global warming, and after he sued the EPA for relief from having to enforce regional smog rules including levels of airborne mercury pollution.
Not only did Oklahoma frackers inject their own wastewater, but they had been happily importing other firms wastewater for disposal after states like Kansas and Arkansas began restricting the practice. In 2015, this amounted to an additional 2.4 million barrels of the stuff, imported and injected into Oklahoma’s subterranean landscape.
But not surprisingly, this was pretty good politics. Pruitt’s campaign manager was oil billionaire, Harold Hamm, who notoriously stated at the Republican National Convention in 2016, “Every time we can’t drill a well in America, terrorism is being funded. Every onerous regulation puts American lives at risk.”
Pruitt and Hamm’s situational ethics aside, evidence is mounting that there is more for Okie citizens to worry about than just a few broken dishes. What they are playing with in Okie health.
1. More than half of our domestically consumed oil and gas comes from fracking.
2. The process involves injecting high pressure, treated water into porous rock strata accessed through horizontal well drilling. Over 100,000 domestic wells have been drilled in the past decade.
3. Ten states sit over vast shale depots including Pennsylvania, New York, Ohio, Maryland, Virginia, West Virginia, Kentucky, North Dakota and Montana.
4. Fracking is complex, multi-stepped, and carries proven risks of air, soil, and water pollution.
5. The water injected during fracking includes sand and a range of chemicals including silicates, acids, and surfactants. The wastewater recovered is contamininated with heavy metals like barium, manganese and iron, radium, and organic compounds lincluding benzene, toluene, xylenes, oil and grease. 95% of that wastewater is injected into deep disposal wells underground.
This week’s JAMA report outlined a range of health concerns including:
1. Asthma: In the states overlying the Marcellus shale (Pennsylvania, New York, Ohio, Maryland, Virginia, West Virginia, Kentucky), asthma patients living near wells were more likely to fill a prescription for oral corticosteroids than control patients living farther away.
2. Silicosis: Workers now must be monitored longitudinally to measure the impact of their respiratory exposure to crystalline silica.
3. Studies are now looking at both neurotoxicity and nephrotoxicity of fracking effluent. This includes manganese impact on basal ganglia and potential association with parkinsonism, mercury effects on dorsal root ganglia and association with idiopathic neuropathy, conversion of mercury to the more toxic methyl mercury by aquatic microorganisms, and altered renal function in those exposed to fracking water.
EPA head Scott Pruitt spends a great deal of time these days flying around on private jets at taxpayers expense. But he’d do well to spend more time on the ground with eyes wide open. Here are a few things he might look to regulating:
1. Fracking fluid spills.
2. Fracking storage wells wells with sub-par mechanical integrity.
3. Injection of fracking fluid into ground drinking water.
4. Inadequate treatment of fracking effluents.
5. Disposal of fracking fluid into unlined and permeable pits.
Or as Will Rogers said, “When you find yourself in a hole, quit digging.”
Tags: earthquakes > EPA > fracking > fracking fluid > Oklahoma > Scott Pruitt > Will Rodgers

 Source: YouTube
Source: YouTube

