Words Matter in Health Reform: Part II – “Single Payer” or “Single Oversight”
Posted on | October 25, 2018 | 3 Comments

Mike Magee
In Part I of this 3 part series, “Words Matter”, we learned that the Canadian system is not technically a “single payer” system, in that provision of insurance (set to national standards) and the delivery of the care is the responsibility of individual provinces, not the national government. A more accurate label for their system would be “Single Oversight/Multi Plan”.
The single authority is Health Canada which provides formalized government health planning as well as insurance standards and oversight. Approximately 24% of the funding for defined “essential benefits” in the Canadian plan is provided by federal taxes, while provincial taxes make up the rest. The national government is the guardian of universality and (often overlooked) simplicity. Providers provide. Provincial government pays. Patients concentrate on health and wellness, and are not plagued by insurance gamesmanship and endless bill bickering on the local level.
On the most fundamental level, the U.S. has no such governmentally-directed, national health planning apparatus.
Service levels and reimbursement vary widely across a endless range of private and public offerings that have devolved into a “free-for-all.”
Employers historically have been heavily involved in offering tax-incentivized health benefits and lately funding their own health insurance plans, though the extent of benefits and number of employers underwriting health care is highly variable and in decline.
Physicians and hospitals in the U.S. are paid according to set rates and formulas for various government sponsored programs like Medicare and Medicaid. Physician payments rely heavily on a relative value scale (RBRVS) pricing controlled primarily by the AMA. But they also negotiate their participation and fee schedules with countless other private insurers. Fee-for-service remains the rule for non-hospital based physicians though over half of all physicians are now employed by large health care firms.
Hospitals rely on bundle payments for episodes of care under the DRG payment system for Medicare, and through mirror offerings from most private insurers. Fraud in coding is not uncommon. Hospital and insurance execs engage annually in often hostile negotiations making long term planning neigh impossible.
Hybrid public/private “Medicare Advantage” (Medicare Part C) plans provide a broader array of services than traditional Medicare in return for patient acceptance of restrictions in physician and hospital choices. Incentive payments to manage complex patients have been subject to abuse.
Supplemental Medicare plans are heavily marketed by associations like the AARP which quietly splits profits with its private partner United Healthcare.
Medicare Part D plans cover a portion of the pharmaceutical costs of Americans over 65. Rates of coverage (governed by tiers) vary widely from one participating insurer to the next, and also increasingly direct the patient to only use approved pharmacy outlets. Rules on individual medicines covered change constantly, drug to drug, making yesterday’s wise consumer decision today’s big mistake.
Long term care and nursing homes receive significant financial support through the Medicaid program. Under the Affordable Care Act, nearly 20 million uninsured Americans received coverage mainly through expansions of state Medicaid in participating states, and are heavily subsidized by federal dollars.
Patient co-pays, co-insurance, and deductibles are ubiquitous in the U.S. system (fewer than 5% of consumers understand these terms), and are further complicated by a series of legal kickbacks and opaque financial inducements and conflicts of interest managed by Pharmacy Benefit Managers (PBMs) – offshoots of insurers, drug manufacturers and retailers – that secretly cross the collusive boundaries between medicine, industry and governmental bodies.
Privatization has become more aggressive of late with moves to syndicate vertical integration (like CVS/Aetna, Cigna/ExpressScripts) and realize outright ownership of supply chains of providers and services that will likely restrict patient choice further without delivering lower cost or resolving patient confusion and complexity.
In short, our health care system, strictly from an economic standpoint, is an intentional complex mess that now consumes 1 of every 5 American dollars.
What are our current assets upon which we might build a comprehensive national health care plan that provides “Single Oversight/Multi-plan” simplicity?
That’s next.
Tags: health authority > health care > health care reform > health reform > single authority > sinle payer
Words Matter When It Comes To Health Reform: Part I.
Posted on | October 22, 2018 | Comments Off on Words Matter When It Comes To Health Reform: Part I.

Mike Magee
Americans views on healthcare reform are evolving. The decade long battle by Republicans to “repeal and replace” Obamacare is fading slowly into the background. Now those same voices who worked so diligently to destroy the plan pledge undying support to prevent denials based on prior conditions, even as they pick away with “skinny plan” intrusions.
Today the greatest risk to continued movement toward universal coverage and rational health planning is nomenclature. To avoid talking past each other, we need to define the terms of this debate while agreeing on common end points.
For example, “universal health care” is an end point goal which reinforces the principle that health is a human right rather than a privilege for the most entitled. “Single payer” is one strategy or tactic for efficiently delivering on the promise of universal coverage. It is something of a misnomer, a term that suggests a comprehensive and centralized public approach to health coverage, but one that may be less than comprehensive and paired with additional private plans which are allowed to emerge on the side. More on that in a moment.
As Americans have struggled to accommodate and absorb a new vision of health care, they have often leaned heavily on other national approaches, notably Canada, with careless approximations rather than laser accurate descriptions of what these systems are or are not.
Let’s take a careful survey of Canada and consider each word. Here are a few key questions with answers:
1. Does Canada have a universal health care system?
Yes. Canada provides equal access to defined “essential health services” to all of its citizens.
2. Who pays for the care?
Canadian citizens fund the care through targeted national and provincial tax payments. Provinces, with some level of federal financial support, are responsible for health planning, budgeting, negotiations with providers, and delivery of quality care.
3. What is the national or federal government’s role?
The 1985 Canada Health Act on a national level requires that each province maintain coverage for “medically necessary” hospital, diagnostic, and physician services. The formal plan must be “publicly administered, comprehensive in coverage, universal for citizens, portable (providing coverage when in other provinces), and accessible (without additional co-pays/user fees).”
Health Canada is also responsible for promoting nationwide health objectives, addressing the needs of vulnerable populations, food and drug safety, and medical device and technology review.
Separate from Health Canada, the nation also maintains the Public Health Agency of Canada which is responsible for public health programming, emergency preparedness, infectious disease prevention, and chronic disease management programs.
4. What is the national versus provincial financial contribution?
The national government funded 24% of the provincial health budget in 2017, while provinces covered 76% of public plan funding. Combined public coverage paid for 70% of total health expenditures, with 30% coming from private supplemental coverage/private pay plans.
5. What major services are not covered by the Canadian plan?
Prescription drugs, dental care, vision care, long-term care/nursing homes, and over-the-counter medications are not covered. These may be covered in part or whole by widespread use of supplemental health plans offered by employers, unions and other organizations.
6. How are physicians paid?
Reimbursement of physicians is based on fees-for-service using bills that are created using the same diagnostic (ICD-10) and procedural (CPT) coding systems used in the United States. Some physicians are private while others are paid on salary by hospital or health care organizations. Physicians are not allowed to “balance bill” – add charges beyond the agreed upon annual government rates. On average, Canadian physicians earn slightly more than their American counterparts ($324K vs. $303K).
7. Do patients pay any “co-pays” or “deductibles” with the Canadian plan?
No. There is no cost-sharing for professional, diagnostic or hospital services. Patients are not involved in billing. Providers bill the government, while patients receive the agreed upon care services.
8. How are hospitals organized and paid?
There is a mixture of public and private hospitals. Private hospitals are mostly non-profit and often have a religious delineation. Hospitals are traditionally paid through annual global budget allotments negotiated directly with the provincial government or through regional health authorities empowered by the provincial government. Recently, certain provinces have begun to explore the use of “activity based funding” to incentivize efficient “through-put” of cases to address wait times in the system.
9. How does the government control health care costs of its plans?
Cost-control strategies are intrinsic to public plan design and include mandatory annual global budgets for hospitals/health organizations, negotiating of physician fee schedules with provincial medical societies, restrictions on approval of new technology, and negotiated drug pricing.
Introductory prices of new patented medicines are set by the government after review of prices in other “reference nations.” Provinces through the Pan-Canadian Pharmaceutical Alliance have negotiated price reductions on nearly 100 brand name drugs and many generic drugs. Direct-to-Consumer broadcast advertising is illegal.
10. How does the government control health care quality of its plans?
The provincial government is responsible for managing the quality of their public plans. Expectations for quality service through Health Canada is clearly defined and largely delegated to the responsibility of provincial physician and hospital organizations servicing their fellow citizens.
A range of quasi-public organizations collect and distribute quality outcomes data to providers for their quality improvement reviews. Accreditation Canada is a non-profit voluntary accreditation service that accredits approximately 1200 hospital and heath service organizations across Canada.
The Canadian Institute for Health Information is a nationally endorsed non-profit established in 1994 and governed by a cross-province board of mostly governmental health executives which oversees data collection from 28 pan-Canadian databases, and manages their analysis and sharing with health system providers. Among other programs, they manage the Canadian Patient Safety Initiative which issues regular transparent reports on preventable patient safety problems in Canada’s acute care hospitals.
11. Is Canada technically a “single payer” system?
No. More accurately, it is a “single payer/multi-plan” system. It is “single” in the sense that “essential services” are required of all provinces, portable coverage between provinces is assured, all tax payers contribute, and rules that govern provider-patient interaction and reimbursement procedures are generally consistent across all provinces.
But, the various plans in each province function largely independent of each other. Specifically, each province determines its own governance structure, negotiates its own annual global budgets and priorities, and customizes certain elements of the program including integration with other social services and protections.
Further, Canada’s national health program covers only 70% of the total health care costs of Canadians. Payment for uncovered services is an individual responsibility, often managed by the purchase of private supplemental health coverage plans.
12. What can we learn from Canada and what have we learned from the Affordable Care Act?
For that answer, tune in next time for Part II of “Words Matter.”
Optum-izing Paul Ellwood’s HMOs.
Posted on | October 16, 2018 | Comments Off on Optum-izing Paul Ellwood’s HMOs.
Paul Ellwood and Richard Burke
Mike Magee
According to Paul Ellwood, often labeled “The Father of the HMO”, the seeds of the Agency for Healthcare Research and Quality (AHRQ) were buried in a report that he delivered to the 34-year-old Assistant Secretary of Health, Phil Lee, in 1969. As Ellwood recalled in 2010, “the emphasis there was on accountability for health care along with evaluating various structural and incentive arrangements for organizing health systems.”
Paul and his Minnesota based associates referred to themselves as “medical ecologists” and realized that health reform in the U.S. would “require a huge cultural shift.” What really stroked their interest was “the notion of measuring health outcomes as a means of determining who and what was effective.”
Ellwood in those early days was both optimistic and naive. In the early 1970’s, he had triggered the formation of an HMO and associated Independent Practice Association (IPA) with the local Minneapolis and St. Paul Medical Society – “a pioneering venture where individual private physicians shared risk and responsibility for the cost and quality of care for a population.”
When the leader of the new venture couldn’t persuade a wayward doctor to address his patients’ excessive length of stay, Ellwood sent over a 32-year-old staff member with “insurance expertise” to correct the problem. The messenger, Richard Burke, was hired, and “undiplomatically kicked the offending physician out of the plan.”
All hell broke loose, but not to worry. Richard Burke went on to start a little venture called Charter Med, a physician practice managed by insurers rather than physicians. A few years later, it was renamed United HealthCare.
While both Ellwood and Burke agreed that measurement could help direct outcomes, Ellwood envisioned a physician dominated system focused on clinical performance, while Burke concentrated on a business directed enterprise where cost-effective choices and and supply chain management fees could lead rapidly to outsized profitability.
For Burke, knowledge was power, but not quite the kind of power his former boss had envisioned. As the new information technology age was just beginning to reveal itself, Burke arguably was the first to realize that mining patient and provider data could be a gold mine. By 1984, he took the company private, and four years later retired – but not before launching Diversified Pharmaceuticals Inc, the first ever pharmacy benefits management firm (PBM).
Burke has remained involved as a strategic force for the company he started. He has been a Non Executive Director of parent company UnitedHealth Group Incorporated since 1977 and has been its Lead Director since September 1, 2017. And insurer United Healthcare has a new sibling, the healthcare IT company called Optum. When it first appeared, analysts thought it would be a future spin-off, instead it is rapidly becoming the center of the United Health Group Universe.
Optum accounted for 44% of UnitedHealth Group’s profits in 2017 ($6.7 billion on $83.8 billion in revenue), and includes data analytics, a PBM, a growing doctor groups in urgent care, primary care and surgical care, chronic care management and behavioral health. Formal Labels: OptumLabs (research), OptumIQ (data analytics), Optum360 (revenue cycle management), OptumBank (health savings account) and OptumCare (care delivery services).
Data management and skimming profits has been especially effective for OptumRx, their newest PBM. In 2017, it generated $64 billion in revenue by fulfilling 1.3 billion prescriptions. Their direct care arm, OptumHealth, is also on a steep upswing, from 60 million patients in 2011 to 91 million in 2017.

Money focused analysts like Burke’s vision of American health care a lot more than Paul Ellwood’s original schemes. Ellwood still holds on to his optimistic (and some would say naive) vision. In a 2010 interview, he reflected, “IT based care should emphasize openness, collaboration with largely free apps based on solid science.”
But Optum is as proprietary as it gets, and as one analyst noted, “…many of their competitors are now mimicking their strategy by trying to buy into some of the same capabilities.” (That would be you, vertical integrators CVS/Aetna and Cigna/ExpressScripts).
The reality is quite stark, if you can believe where OptumLabs has focused its’ energy. It’s still on data and disruption, as it was for Richard Burke in 1976, but faster, smarter, and more profitable – for them, not for you. Here are their three major concentrations:
1. Machine learning.
2. Artificial Intelligence (AI)
3. Natural Language Processing.
Tags: health care costs > health information > health measurement > health outcomes > hit > Optum > Paul Elwood > Richard Burke > UHC > United Health Group > United Healthcare
A Disturbing Pattern: From OxyContin to Vitamin D
Posted on | October 5, 2018 | 6 Comments

Mike Magee
Winter is fast approaching, a time to bundle up and a grim reminder for many to load up on Vitamin D. Osteoporosis, osteomalacia, rickets, fragile fractures – there’s no end to the misery awaiting you if you fail to take this supplement. Or so we’ve been told, by many every-day doctors with the same assurance as they once used to explain that “pain is the 5th vital sign” and OxyContin is non-addictive.
If you’ve been oversold on Vitamin D, you can thank AMA Federation member, the Endocrine Society, and one specific Boston endocrinologist. Oprah loves this guy. So does Gwyneth Paltrow and Dr. Oz. And so do the drug makers, the blood testers, and the owners of tanning salons whose trade association, the Indoor Tanning Association which disbanded in 2017 gave BU $150,000 from 2004 to 2006 specifically to fund his research.
His bio says that “He served as the chair for the Endocrine Society’s Practice Guidelines on Vitamin D, authored more than 400 peer-reviewed publications, and has written more than 200 review articles, as well as numerous book chapters.” What it doesn’t say is that he is credited for almost single-handedly launching the “billion dollar vitamin D sales and testing juggernaut.”

Michael Holick, MD, PhD is an endocrinologist from Boston University. He chaired the Endocrine Society’s clinical guidelines publication in 2011 that concluded that “vitamin D deficiency is very common in all age groups” and that normal levels should be between 30 and 100 nanograms per milliliter. That was only months after an IOM consensus group concluded that “all individuals meet their needs at intake levels provided in this report” and that 20 nanograms per milliliter were more than enough.
As with the new tighter levels for cholesterol, Holick’s team greatly expanded the list of Americans who were vulnerable and would require treatment. The new Endocrine Society pronouncement targeted the majority of U.S. population for testing, and gullible physicians were more than happy to comply. Quest and LabCorp immediately adopted Holick’s normal level of 30, making an estimated 80% of the adult US population deficient of Vitamin D. By 2016, doctors were ordering more than $10 million worth of the tests at a cost of $345 million, with patient co-pays varying from $40 to $235 dollars.Vitamin D tests were now the 5th most common test reimbursed by Medicare.
Since then, here’s what we’ve learned about Dr. Holick:
1. He has been a consultant for Quest for over four decades and is still paid $1000 per month.
2. Between 2013 and 2017, he received $163,000 from Sanofi-Aventis, Amgen, Roche, and others.
3. He has described “tanning beds” as a “recommended source” of vitamin D.
4. Recent studies have found no link between low levels of Vitamin D and fractures in elderly, heart disease or cancer.
5. However, studies have revealed that levels of 50 nanograms per milliliter or above carry an increased risk of death. The United States Preventive Services Task Force in 2018 recommended that older Americans outside of nursing homes not take vitamin D supplements to avoid falls.
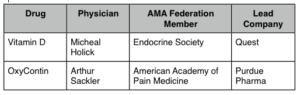
There will always be Sackler’s and Holick’s in medicine. That’s probably unavoidable. But overselling opioids or vitamin D tests wouldn’t have been possible without AMA specialty society cooperation and an army of naive physician prescribers.
Endocrine Society: 2018 Corporate Liaison Board:
NEJM Weighs in on Preventing Gun Violence
Posted on | September 27, 2018 | 1 Comment
In an article this week on prevention of gun violence , Garen Wintemute offers this list of solutions:
ACTIONS TO PREVENT FIREARM VIOLENCE
- Improve background-check policies
- Require background checks for private-party transfers
- Require state and local agencies to report prohibiting events
- Fully implement the existing federal background-check requirement
- Clarify definitions of prohibiting events
- Strengthen enforcement efforts
- Consider a permit-to-purchase approach
- Prohibit release of firearms until background checks are completed
- Enact gun-violence restraining order policies
“The Commitment to Mutuality is Fragile in the U.S.”, Says Berwick.
Posted on | September 25, 2018 | Comments Off on “The Commitment to Mutuality is Fragile in the U.S.”, Says Berwick.

Mike Magee
Earlier this month Donald Berwick published a thoughtful article in JAMA titled “Politics and Health.” It touched on a range of themes that I addressed in a speech in 2005 at the Library of Congress.
In that speech, I said, “There is a growing political disconnect between those who make health policy and those most affected by health policy. While the former continue to reinforce silos and the status quo, the latter seek broad, fundamental and comprehensive reform. Such reform might include expansion of insurance coverage, realignment of financial incentives toward prevention, increased reimbursement of physicians and nurses for team coordination that includes home health managers, support for early diagnosis and screening, and expansion of education and behavioral modification for individuals and families.”
Berwick’s current commentary touches as well on this disconnect. He says, “Presidents, governors, senators, and congressmen take no oath to serve patients. Their oath is to a broader, vaguer duty: to uphold the Constitution. Nonetheless, their choices invade the clinical arena continually.”
The disconnect is fueled by money and power. The Medical-Industrial Complex now consumes 1 in 5 dollars, and clearly its financial objectives and the needs of everyday Americans are often at odds. As Berwick notes, “A nation that values entrepreneurship and protects private profits cannot expect that those motives will fail to engage the enormous financial opportunities through every possible channel of influence. The fragmentation of ownership, governance, and oversight of US health care makes it possible for a vast industry of political pressuring to flourish.”
Adding fuel to the fire:
1. Disagreement over state versus federal prerogatives.
2. Lack of trust in science in the era of Trump.
3. Hijacking health care in support of religious ideology.
4. An American mythology that over weights individualism and self-determination.
Without saying it, Berwick suggests that the health care battle is really a cultural battle. In his words, “Politics enters health care through attitudes toward solidarity…Government, and therefore politics, is the avenue for the expression or the negation of that sense of solidarity.”
Berwick suggests with some deference that “the commitment to mutuality” is “fragile in the United States.” He places the onus on physicians (and health professionals) subtly suggesting they lead the way stating: “The basic credo of physicians—to put the interests of patients before their own—at its best reflects a form of solidarity: that those who are fortunate are duty-bound to help those who are less fortunate.”
Polls leading up to the 2018 mid-terms are now clearly demonstrating that the majority of Americans agree that when it comes to health care in America, Berwick is right. We are all in this together.
Tags: Donald Berwick > physician code > politics and health > universal health care
A National Disgrace: Immigrant Children Imprisoned – # Growing
Posted on | September 21, 2018 | Comments Off on A National Disgrace: Immigrant Children Imprisoned – # Growing




