Scheining A Light On Health Reform
Posted on | August 5, 2019 | 2 Comments

Mike Magee
In 2004, Edward Henry Schein, a professor at the MIT Sloan School of Management, advanced a theory and scheme for understanding the contradictions that exist in organized culture.
His system shined a light on obvious conflicts between our stated values, our actual behaviors, and the hidden assumptions, biases and prejudices that sub-consciously anchor those behaviors.
This week, the nation witnessed the harsh realities of the Schein schema in full display. As one commentator described it, “Cultures are dysfunctional when the underlying assumptions don’t line up with the values we claim to hold dear. For a very long time, America was seriously out of alignment. But we slowly worked to change the underlying assumptions. It became unacceptable to refer to black people by racist names, to utter racist tropes, to run for office on racist themes. It took decades, but we got to a place where it generally wasn’t tolerated, in board rooms or in bars. Leaders who said racist things were often ostracized, forced to apologize, to say publicly they were deeply sorry that they acted in a way that offended our culture….the control rods of our culture…reduced the danger…Our President …lifts the control rods for a deeply cynical purpose: to harness the political energy unleashed.”
These actions are clearly reckless and disqualify Trump. His removal in 2020 is no longer optional if we as a people are to have any hope of aligning our values with our behaviors. But even with Trump gone, the road ahead will require remarkable leadership and a guiding vision. This is because the “control rods” have been lifted at a moment of great change (a moment when technology, globalization and environmental calamity are colliding) and at a time when a sizable portion of our population are at grave economic risk.
While the vast majority of growth in assets in the past three decades went to the top 10% in the US, debt increased by $9 trillion with ¾ of the debt issued to the bottom 90% of American families. For the top 1% during this period, median net worth grew 178% to over $11 million. For the rest of us, earnings have been flat while housing prices have increased 290%, four year college tuition has soared 311%, and average per-capita health care expenditures has risen 51%.
The challenge then must be viewed on two planes: one economic, and the other cultural and value based. These two arenas are far from unrelated. As our hyper-competitive form of capitalism has squeezed out any notion of national solidarity, the gap between the “have’s” and the “have-not’s”, and the visual displays of cruelty and savagery in Texas and Ohio, in Trump arenas and cages filled with children, forces us to acknowledge a modern day reality: We do not like, nor can we accept, what we have become.
To put this genie back in the bottle, we must simultaneously address the nation’s values and economics. The quickest, most direct pathway is now through universal health coverage. Not only would this offer the opportunity to distribute wealth more equitably, but it would also offer the country the opportunity to put Professor Schein’s theories to practice by acknowledging our mistakes of the past, and working anew at aligning our actual behaviors with our stated values of compassion, understanding and partnership.
The Preamble and Health
Posted on | July 22, 2019 | Comments Off on The Preamble and Health
Mike Magee
As a matter of self-defense, I and many other American citizens have been exploring our origins and the stated purpose of our country, its Constitution and ideals, as much in part to reassure myself that most Americans are good and decent people, not perfect but also not intentionally racist, misogynistic or cruel in the extreme.
Recently I have been focused on the Preamble to our Constitution. It is a single sentence that carries no legal weight. But rather, it is intended to be a succinct introductory statement of the principles at work in the full Constitution.
It says: “We the people of the United States, in order to form a more perfect union, establish justice, insure domestic tranquility, provide for the common defense, promote the general welfare, and secure the blessings of liberty to ourselves and our posterity, do ordain and establish this Constitution for the United States of America.”
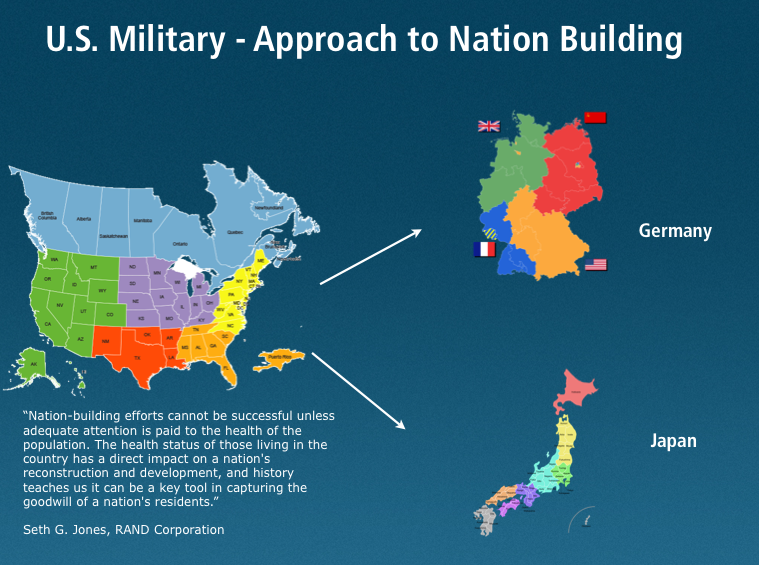
This, in a nutshell, is the American dream of self-governance in an imperfect world of constant flux, of good and evil, of incredible complexity and endless choices. It is a world of accelerating change, where we are forced to adapt and evolve, or be left behind. And yet, it is certainly no more complex than the world vanquished Germans and Japanese faced in 1945 when their defeat meant literally that they would need to start all over again. With the aid of American taxpayers, and the Marshall Plan, they embraced a common starting point – universal health care.
Warfare is not the only disrupter that can lay waste to a nation. In a short two decades of this new century, technology, global markets, and climate change have left the American experiment in all manner of disarray. Justice, tranquility, defense, welfare, and liberty itself have been undermined. Our prime-age workers in the bottom 60% have seen no real income growth in four decades. During this span, the income of the top 10% has doubled, and the income for the top 1% has tripled.
Our nation has not figured out how to get along economically with our market equal, China. We have no “rules, norms, or laws” to protect trust and truth in a world of social networks, cybertools, and cyberbullies. Longer lifespans have until recently translated into multi-generational complexity and competition for resources. As one expert short hands it, we have moved from a “work, learn, retire” model to a “learn, work, learn, work, learn, work” survival mode.
We are desperately behind the eight ball here, and need to listen to our own Preamble and our own history. It suggests that, in establishing our Constitution, we continually must determine how best to promote and maintain a healthy nation filled with healthy citizens – mind, body and soul.
The 2020 election is an opportunity to reclaim self-governance, to plan, to work, to build together. Universal health coverage, as we learned in the reconstruction of Germany and Japan, is not the only platform from which to launch a recommitment to our common future, but I would argue, it is a logical starting point to pursue “a more perfect union” during these turbulent times.
Reaching for Health Equity.
Posted on | July 18, 2019 | 1 Comment

Mike Magee
This past week, New York Times columnist, Thomas Friedman, laid out his concerns for our nation in the starkest terms. He defined the current Trumpian Republican leadership as “an overthrow of all the norms, values, rules, and institutions we cherish”, and asked Democrats who have been sparring with each other to “please, spare me the revolution! It can wait.”
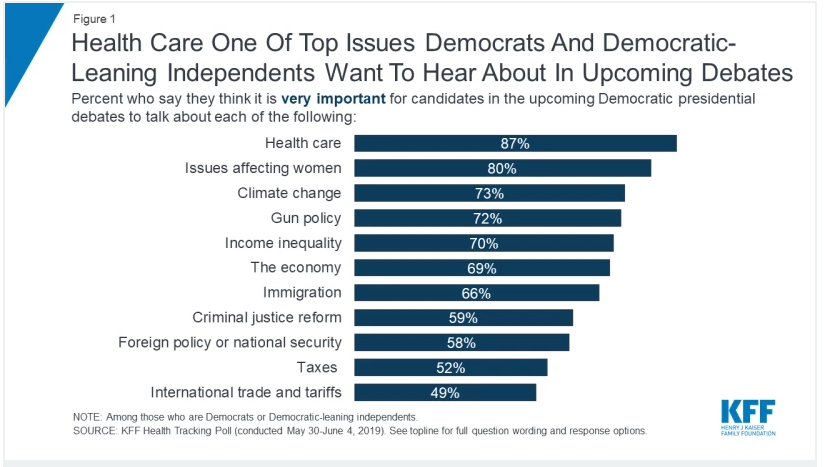
Friedman sees the 2020 election as “a vote to save the country”, and lays out two simple priorities to prevail: 1)national unity and 2) good jobs (a job that can support a family and comes with health benefits).
As the “financial and carbon debts for our kids” rise in tandem with this weeks record temperatures across 2/3’s of our nation, it’s easy to go along with Friedman’s and Speaker Pelosi’s cautious approach, and status-quo (just one more time) to avoid what most would agree could be a Trump 2nd term-induced disaster for our nation and our planet.
But some – including me and Warren Buffet – would argue that the “government enriches the soil and entrepreneurs grow the companies” mantra, at least when it comes to health care, simply is no longer enough, and extends the appetite of what Buffitt calls “the tapeworm on America’s economic competitiveness.”
With one in five dollars already going to health care, a wasteful system that denies care as it bankrupts vulnerable citizens, and restricts upward mobility by trapping workers in jobs they hate for fear of loosing health insurance, supporting reasonable public safety net expansion is not radical – it’s sensible.
The shortest road to national unity is freedom from fear – fear of pain, fear of illness, fear of financial ruin, and fear of societal disruption in a state unable to embrace the basics of common decency and sound public health policy.
Growing income disparity, arguably, is our greatest threat. And the single, most effective move toward addressing it, would be accomplishing the original intent of the ACA, and assuring all of our citizens have comprehensive health insurance – through one pathway or another.
I’m with Friedman and Pelosi that, under the current circumstances, we can’t be reckless – for example forcing those who have it and like it out of their employer health plans. But we can offer them a better option – and many employees and employers will voluntarily choose that pathway.
We can also reassert appropriate checks and balances that disrupt what is now a criminal and collusive medical-industrial complex that has as much chance of adopting responsible self governance as does our current president in adopting virtue-driven and inclusive leadership.
Tom Friedman is correct in suggesting that we must be cautious and wise, but that does not mean that we must cower in the face of changes that are entirely reasonable and long overdue.
“Top 100” Vine Voice Review: CODE BLUE “a landmark book…required reading for all Americans – excellent!”
Posted on | July 13, 2019 | Comments Off on “Top 100” Vine Voice Review: CODE BLUE “a landmark book…required reading for all Americans – excellent!”

Vine Voice Reviewers are among the most respected in the book industry. To gain entrance as a “Top 100” reviewer takes it up another notch. Chicago’s Becky Brooks has earned this elite status. Here’s what she says about CODE BLUE: Inside the Medical-Industrial Complex.
“First of all – this is a landmark book and should be required reading for all Americans on a topic they probably think they understand but really do not. Forget what you think you know about why healthcare, insurance, and drugs cost as much as they do. This book tells the tale in easily digestible detail, providing the historical and ongoing perspective to illustrate how things evolved to the unacceptable place they are today.
I have read several books concerning the state of health care in the US and other countries and none of them has covered the subject so objectively and factually.This is probably due to the fact that the author was/is a healthcare professional, a doctor who has also worked for big pharma. Not technically a whistle-blower he does present the facts about modern health care and has come to the conclusion that is there is a better way.
Eisenhower famously said after the conclusion of World War II, “ beware the military- industrial complex”, and rightfully so.This concentration of corporations, government, partisan politics, profits, and lobbying all acting together has essentially shaped a lot of the modern US today. He makes the correct point that now we have to deal with this same type of concentration the “ Medical Industrial Complex”.Big Pharma, insurance companies, doctors, all acting in their best interests: profits and cutting costs rather than cures and patient welfare. They have changed the whole approach to healthcare and so much privatization has not lowered costs nor improved preventative care or cures.
It is ironic that countries like Germany and Japan have all -exclusive, low cost, quality healthcare because after the war when we were rebuilding these countries under the Marshall Plan, we realized the social structure had to be built back up as well as the bombed buildings. We put universal type health care in place which still thrives today.
I hope this review piques your interest to read this book – there are many facts ( how the AMA came about, politics and back room deals to move things forward) that are eye-opening. Undeniable facts. The Medical Complex has become so big and powerful it is extremely difficult to change things – but as the author state we must. Life, liberty , and the pursuit of happiness certainly must not exclude the right to affordable and accessible healthcare. Access to healthcare is not a privilege.
Think of this book as a wake up call, much like Rachel Carson’s “Silent Spring” warned of the unpublished dangers of pesticides. It’s that big of a subject, that big of a problem, and that important a book.”
Thanks for reading my review
Becky Brooks
Medicare-For-All (Who Want It) is a Carrot that needs a Stick.
Posted on | July 3, 2019 | Comments Off on Medicare-For-All (Who Want It) is a Carrot that needs a Stick.
Mike Magee

On June 27, 2019, Pete Buttigieg was asked whether he supported Medicare-For-All. He responded, “I support Medicare for all who want it.”
In doing so, he side-stepped America’s Achilles heel, the controversial debate over shifts of power from states to the federal government. He was suggesting that times have changed and that he might prevail with Red States nipping at his heels.
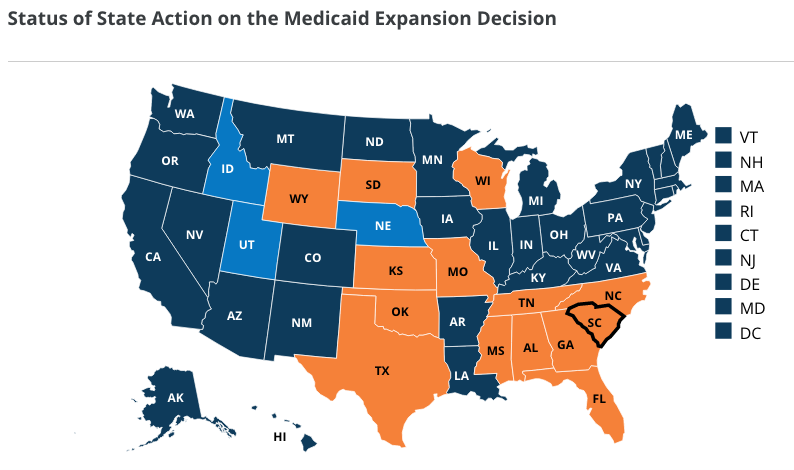
Two reality maps challenge that assumption. The first is a map produced by the Kaiser Family Foundation cataloging the status of ACA Medicaid expansion in the US. The current score card includes 36 states that have or will soon participate, and 14 hold-out’s. This latter group, as has been so well-expressed by former Ohio Gov. John Kasich in the past, has chosen to vote against its own state financial interests and the servicing of its states most vulnerable citizens in the interest of keeping the federal government out of their business.
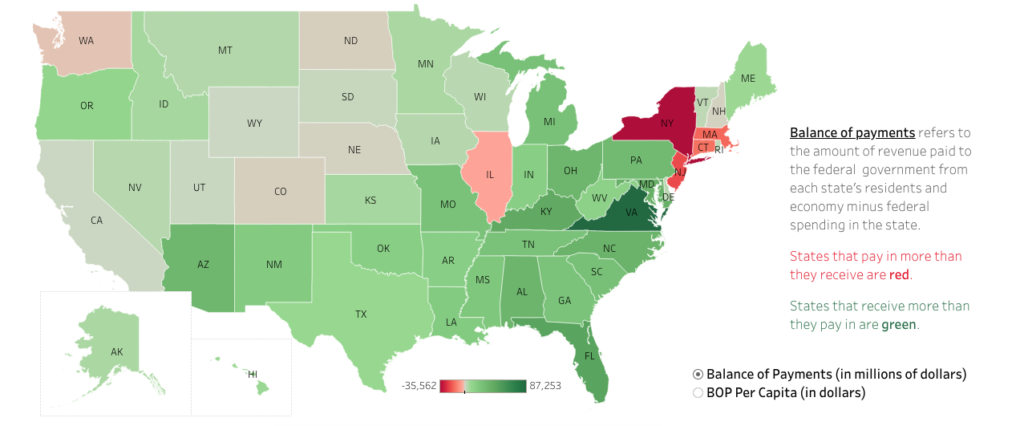
The second map comes courtesy of the Rockefeller Institute of Government and demonstrates a footprint with significant overlaps to the KFF version. It measures the amount the states contribute to the federal government through taxpayer dollars against the amount they draw off the federal government in benefits. This lays bear the truth that Red States rejection of federal underwriting is highly selective and politicized.
As I outline in my new book, “CODE BLUE: Inside the Medical Industrial Complex”, at the close of WW II we diverged from both allies and foes and went all in on cures over care, and profit over planning. Seven decades later leaders of medicine, pharmaceuticals, insurance, hospitals, and medical research have coalesced into a Medical-Industrial Complex that has dealt everyone in – except the patient.
A status quo that favors and protects states rights maintains needless complexity – on purpose. The more complex, the less we understand, the more we pay. In addition, if you’re in the business of maintaining the status quo in American health care, it pays to be financially strong enough to simultaneously field lobbying forces in all 50 states and Washington, DC as well. It’s also helpful if your organizational structure is based on state and county societies – say, like the AMA. And if your government relations armies are willing to cross sectors and collusively plan resistance strategies, all the better.
Mayor Pete is right in suggesting that Medicare, extended to all comers, will have little difficulty competing with private plans and their purposeful complexity. But to achieve the desired outcome of high quality, low variability and efficiency, our nation requires an empowered majority that clearly expresses “enough is enough.” Otherwise the self proclaimed “Grim Reaper” Senate Majority leader will continue to determine all of our futures.
“Medicare-for-all (who want it)” can not stand alone. It must be anchored in shared principles including:
1. Less is more. Insurance Simplicity = Savings and Improved Quality and Performance. .
2. Health = Full Human Potential (not the elimination of disease). Innovative research is great, but it is no substitute for national health planning and public health programming.
3. The Public Option must reinsert appropriate checks and balances. The integrated career ladder that currently entangles academic medicine, pharma, insurers, hospitals and government regulators is a cesspool of conflicts of interest and no longer deserves safe haven.
Why CODE BLUE is in Staffers Bags in June, 2019.
Posted on | June 18, 2019 | Comments Off on Why CODE BLUE is in Staffers Bags in June, 2019.
Memorializing Three Soldiers
Posted on | May 27, 2019 | 1 Comment
Mike Magee
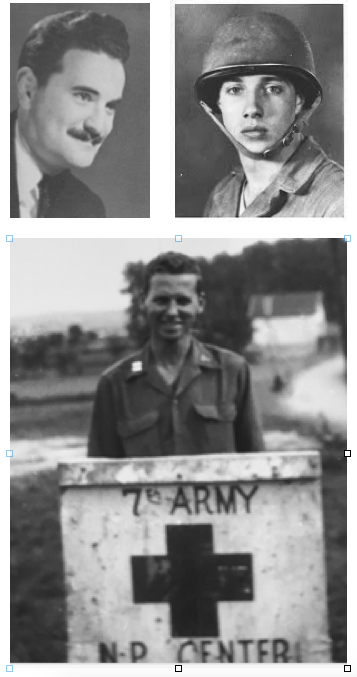
CODE BLUE (Grove/2020) began four decades ago in the noontime conference room of Colin (Tim) Thomas, M.D., chairman of surgery at the University of North Carolina, where I completed my surgical training in 1978. Tim’s pre-op conferences exposed us to his broad knowledge and understanding of medical history and its role in shaping compassionate and empathetic health professionals. Some two decades later, Eli Ginzberg PhD, the legendary Columbia health economist, generously guided me down the same pathway, and pointed me toward World War II as I struggled to understand how and why the physician had become so entangled in the Medical-Industrial Complex.
My father, William P. Magee, M.D., who was my professional and personal role model, died of Alzheimer’s disease in 1998 during my early tenure at Pfizer. He was a decorated captain in the Medical Corps of Patton’s 7th Army in Europe, one of Dr. William Menninger’s “30 Day Wonders”, trained to manage psychiatric casualties in battle zones during the war. Seeking his war records at Eli’s urging triggered a decade long exploration, reinforced by a two year, Viagra induced association with one famous World War II casualty, Senator Bob Dole.
During my travels with Dole, it became clear that my father and Bob likely crossed paths many years ago. Dole passed by stretcher through Southern Italy evacuation hospitals that my father was helping to staff prior to his participating in the invasion of Southern France.
The 5-tier “chain of evacuation” which spanned the distance between battlefield and stateside specialty hospitals saved the life of Dole and countless others. My father worked that chain, and Eli Ginzberg helped design it. These three – the military doctor, the injured soldier, and the wartime administrator – were my silent guides through the early years of unraveling the story of how American health care came to be the global outlier it has become.
As we depart another war zone in the summer of 2021, I remember each of them, and their service to this country, with gratitude.


