The Real Arthur Sackler. Part 2: MIC Poster Boy.
Posted on | September 24, 2019 | Comments Off on The Real Arthur Sackler. Part 2: MIC Poster Boy.
Mike Magee
Series Note: This 5-Part Series will run from September 23rd to September 27, and then be available as a single document under Hcom Resources.It is based on original research in CODE BLUE: Inside the Medical-Industrial Complex.
In Part I of The Real Arthur Sackler, I reviewed his official narrative which had been carefully scrubbed over three decades by New York’s finest public relations experts. But the truth diverges dramatically from the varnished version, and reveals a rich kid who sets his sites early on becoming the marketing poster boy for a wildly profitable Medical-Industrial Complex (MIC).
Arthur Sackler was born in 1913, the son of immigrants, his father from the Ukraine, his mother from Poland. They lived in Brooklyn. By all accounts their son, who attended the famed Erasmus Hall High School, was both intelligent and industrious.

A statue of the school’s namesake was erected in 1930 and sits in the school’s courtyard. An accompanying inscription, which likely inspired the young Arthur, graduating that same year, read, “Desiderius Erasmus, the maintainer and restorer of the sciences and polite literature, the greatest man of his century, the excellent citizen who, through his immortal writings, acquired an everlasting fame.”

By 1937, (even while narratives suggest he was functioning as a significant source of financial support to parents, siblings, and self), he completed both college and medical school in record time, and married his well-to-do first wife, Else Finnich Jorgenson. Three years later, in 1940, after completing an internship at Lincoln Hospital, he departed clinical medicine, adjusting his career path and was already wealthy enough to begin to seriously collect art.

He was now a pharmaceutical managing director, and head of the Medical Research Division at Schering Corp., a American based subsidiary of German parent, Schering A.G., established in the early 1800s by the German apothecary Ernst Schering. Sackler’s American division was established in 1938 “in preparation for its assignment of supplying and holding the foreign markets of Schering A.G. for the duration of the anticipated hostilities”. Germany was on the march and FDR was preparing for war, and Schering wanted to protect its supply chain exports to the U.S.
Young Sackler’s role as head of the Medical Research Division included medical affairs. That year, on behalf of Schering Corp, he presented an endowment check at the Annual Convention of The Association of Medical Students. The funding was to fully support a new award program called “The Schering Award”, to encourage student interest in the burgeoning field of endocrinology – central to Schering current product line.
Two years later, the award and Schering Corp. were gone, seized by the US government with other “German interests”. It would be another ten years before the government released the 440,000 shares of Schering stock being held, and allowed the company to once again function independently.
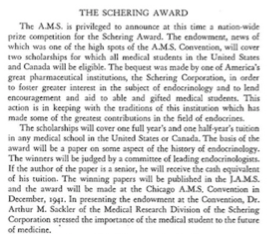
Arthur used that decade well. With Schering gone, he joined the William Douglas MacAdams Advertising Agency in 1942, and by 1947 gained a controlling interest in the firm. At the same time, with a healthy understanding by now of medicinal chemistry, he witnessed a stream of over 1 million psychiatric casualties returning from WW II and inhabiting overflowing mental hospitals stateside, and decided psychiatry was the land of opportunity.

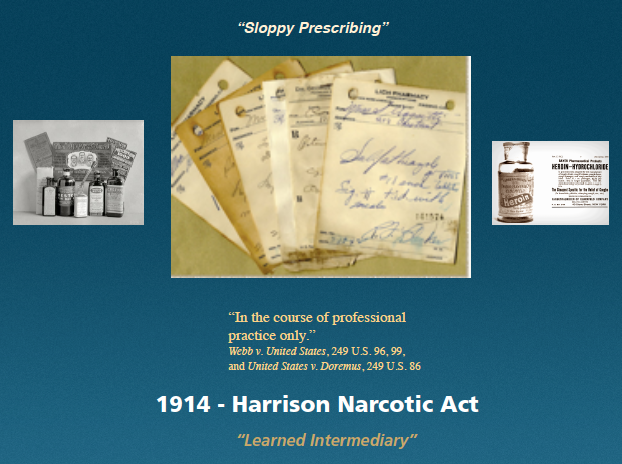
He enrolled in the New York residency program at Creedmore Mental Institution on Long Island. The specialty was getting a huge boost from the war effort. U.S. Army head of Psychiatry, William Menninger, was systematizing the treatment of “Shell Shock” including the liberal use of barbiturates. His playbook, Medical 203, would become the basis of DSM 1 in just a few years, and launch the medicalization and pharmacologic treatment of mental illness. Name it, then treat it.
By 1949, Arthur not only controlled his own Medical Advertising Agency and had completed his training, but had now established, with his two brothers, Mortimore and Ray, the Creedmore Institute of Psychobiological Studies. With access to 7000 plus in-patients, there was no shortage of human subjects. Experimenting with a variety of agents, including sex hormones and histamine, on patients with psychosis, Arthur and his kin began to churn out papers advancing their theories on the biologic basis of treatment for psychiatric illness, and publishing the same in home-made scientific journals which celebrated his brillance.

His business success was not mirrored in his personal life. By 1949, he had divorced his first wife (though secretly maintaining her as a hidden silent business partner), and married his second wife, Marietta Lutze, the third generation manager of the German Pharmaceutical firm, Dr. Kade. All the time, Arthur had been ramping up his art collecting, now focused heavily on Asian artifacts. And as luck would have it, he was flush with cash. The Antibiotic Era was about to come into full bloom.
Tomorrow: The Real Arthur Sackler. Part 3: Pfizer’s Agent of Record
The Real Arthur Sackler. Part 1: The Official Narrative
Posted on | September 23, 2019 | Comments Off on The Real Arthur Sackler. Part 1: The Official Narrative

Mike Magee
Series Note: This 5-Part Series will run from September 23rd to September 27, and then be available as a single document under Hcom Resources. It is based on original research in CODE BLUE: Inside the Medical-Industrial Complex.
The official narrative, as it exists today, oft repeated by premier medical and cultural organizations, who maintain schools, exhibit halls, and colloquia that bear his name, features:
1. A remarkably industrious boy who, from an early age, supported his parents (who lost everything in the Depression), put himself through college and medical school at NYU, doing the same for two younger brothers who sought medical school overseas to escape prejudice.
2. A boy who grew up in “hard times”, whose parents were grocers in Brooklyn, chose medicine as a vocation at the age of four, but whose passion drew him more than equally to Art, pursuing art and sculpture lessons as a teen, and taking courses at New York’s famed Coopers Union while attending college and funding the family besides.
3. A committed physician and researcher who generated 140 science related papers, dealing primarily with exploring biologic approaches to psychiatric illness in the 1950’s.
4. A remarkably prolific philanthropist focused on brand name institutions in Medicine and the Arts.
5. A very successful business man, whose extended family fortune was pegged in 2015, at $14 billion, 18 years after his untimely death at age 73 from a heart attack.
Yet, the details that tie Arthur M. Sackler to the Man-made Opioid Epidemic, and the well established tactics that helped consummate the Medical Industrial Complex in the second half of the 20th century are largely hidden from public view. What is the full picture?
The answer tomorrow in The Real Arthur Sackler. Part II: MIC Poster Boy.
Retail Pharmacy: The Nucleus of the Pharmaceutical Industry. Part 3. The Prescription.
Posted on | September 10, 2019 | Comments Off on Retail Pharmacy: The Nucleus of the Pharmaceutical Industry. Part 3. The Prescription.
Mike Magee
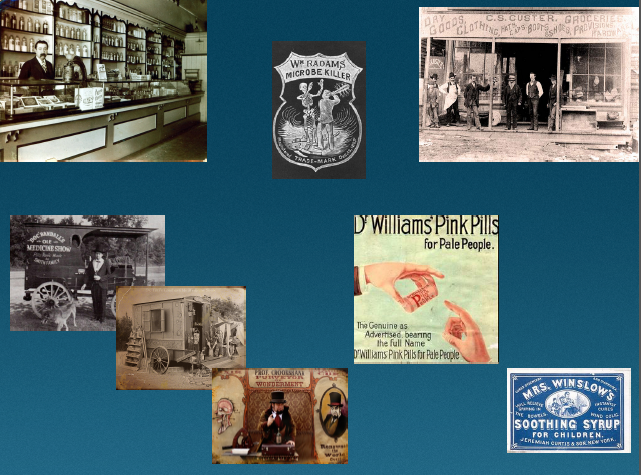
William Radam’s “Microbe Killer”, and other variations of mistreatment, with or without healer negligence, were mainly what instigated two hundred and fifty physician delegates from 28 states to coalesce at the founding meeting of the American Medical Association in Philadelphia, Pennsylvania on May 7, 1847. The meeting had been triggered by a motion from Nathan S. Davis, a young New York physician and member of the New York Medical Association in 1845, calling for a national convention. At that 1847 meeting, the delegates approved the establishment of the organization, elected Nathaniel Chapman its’ first president, approved a Code of Ethics, established nationwide standards for preliminary education and the degree of MD – and then called it a day.
But then, over the next 24 months, this young organization, according to its official history, “analyzed quack remedies and nostrums to enlighten the public in regard to the nature and danger of such remedies”; “recommended that the value of anesthetic agents in medicine, surgery and obstetrics be determined”; “noted the dangers of universal traffic in secret remedies and patent medicines”; and “recommended that state governments register births, marriage and deaths”.
Of course they also painted their competitors, homeopathic physicians and osteopathic physicians, with a broad negative stroke. Over the next half century, homeopathic physicians would disappear and Osteopathic Medicine would be repeatedly labeled as a “cult”. It would take over 100 years for the AMA to grudgingly agree to the equivalency of an M.D. and a D.O.
But for the young immigrant cousins, Charles Pfizer and Charles Erhardt, who arrived in Brooklyn in 1849, the timing couldn’t have been better. They intended to produce chemicals and medicinals that were safe and effective. And they saw these new physicians, certified and focused on routing out their “quack” competitors as an asset, a “learned intermediary” that would deliver their product reliably and with implied professional endorsement to patients far and wide. What could be better?
The sales vehicle that would close the deal, a prescription, became commonplace after 1914, when the Harrison Narcotic Act “required prescriptions for products exceeding the allowable limit of narcotics and mandates increased record-keeping for physicians and pharmacists who dispense narcotics.”
That single stroke of the pen had enormous ramifications that we are arguably still negotiating today. The boundaries it established included: separation of duties for physicians and pharmacists; separation of disciplines of pharmacy and pharmaceutical manufacturer; legal cover from some liability for pharmaceutical manufacturers, who once their drug is “approved” by the FDA, hand it – and its liability – over to the physician “learned intermediary” to prescribe; separation of product that exists behind the counter and requires a prescription, from product that is “over the counter”; and separation of product that is still under patent protection from “generic” product which is not protected.
Of course the full ramifications of the 1914 Harrison Narcotic Act were yet to play out. Most of the issues above were only addressed by case law in the later part of the 20th century. Some remain evolutionary and unresolved today. What was obvious at the time was that the AMA was “in charge” of Medicine in America, at the top of the heap. They were aggressive and organized. Through the Flexner report, they would soon radically shrink medical schools and hospitals, forcing the survivors to tow a “quality line” that they alone had defined. They would jealously protect the “right to prescribe”, and in so doing hold competing practitioners, and increasingly educated patients, at bay for most of the next 100 years. They would turn a blind eye to “sloppy prescribing” and willingly accept the ad dollars and physician masterfile data revenue from pharmaceutical companies that would ignite a deadly opioid epidemic a century later.
And they would do all this with the very active support of Charles Pfizer, Charles Erhardt, and their pharmaceutical colleagues, who would grow very, very rich in the process.
Retail Pharmacy: The Nucleus of the Pharmaceutical Industry. Part 2. Crossing The Pond.
Posted on | September 7, 2019 | 1 Comment
Mike Magee
By the 18th century, in Germany, England, France and Switzerland, says one British historian, “a man practicing pharmacy, whether apothecary or chemist and druggist”, saw his retail operation as the cornerstone of a potential wholesale gold mine.
What is it they produced back then? Well at least in Britain, the answer is, quite a lot of what is affectionately termed today “little technology”. From the same British historian, “Pills and boluses could be made by hand, tinctures by the simple process of maceration or the slightly more complex one of percolation, infusions were more than making a cup of tea, and ointments merely used mortar and pestle. Few chemists and druggists were content with just dispensing, but developed what has been termed their ‘own lines’, that is the pharmacists own formulation for a soothing cough mixture, a worm eradicator, an ointment for scabies, but not too griping purge. Many hoped to make a fortune.”
So in one sense, Mr. Jones’s philosophy of never leaving a penny on the floor, undeveloped, was an inherited value dating back a century or two. These were versatile and imaginative entrepreneurs, experimenters with high productivity, if not uniform quality. One pharmacy in Birkenshaw, Yorkshire, had a handwritten formulary that included 534 discreet formulas – 316 medicinal, 69 cosmetic, 68 veterinary, and 81 “domestic”. Among the lot were compressed tablets, cold creams, lotions, essence of smelling salts, powders of all types, and brandy. But of course, there were other offerings considerably more exotic like cockroach bait, glove cleaner and non-mercurial plate powder.
Simple discoveries in delivery systems expanded the market. Cocoa butter introduced in 1852 launched a worldwide surge in suppositories. The soft gelatin capsule opened all new possibilities in 1834. Subcutaneous injections followed in 1855. By then, some medicines were described as patent or proprietary, but most were simple ‘secret formula’ concoctions that were not registered. As one expert noted, “The ‘quack’ medicines would have had little, if any, therapeutic value, but then neither had most of those prescribed by physician or surgeon apothecary; indeed there was often little to tell between them. The ‘patent’ medicine trade at least had the merit of passing on the knowledge of how to manipulate equipment and mix ingredients in bulk.”
These larger scale and more methodical chemists became increasingly prominent in Europe, and to a much lesser extent in America, in the second half of the 19th century. They produced three general types of products – those derived from simple compounds of vegetable substances (examples being ginger or aloes); those generic substances listed in the official country’s Pharmacopoeia, a document of “real medicines” carrying the imprimatur of the country Medical Society (like morphine and quinine); and those that were being developed increasingly according to new industry standards which emphasized systematic chemical research and laboratory development (such as new sera and vaccines).
Prominent as leaders of the 3rd group in 1880 in Britain was Burroughs Wellcome. While London based, it was the brainchild of two American entrepreneurs, Silas Burroughs and Henry Wellcome. Marketers at heart, they were the originators of sales visits to doctors offices and free samples left behind – a practice that would a century later be tangled up in a contentious debate over conflict of interest and direct advertisements to patients themselves.
Flowing in the other direction of Burrough and Welcome were chemists and scientists like German immigrants Charles Pfizer and Charles Erhardt who saw immense opportunity in America as this energetic nation took its first transformational steps into the Industrial Age. Still others, like fellow German immigrant Willliam Radam, saw in America the “Wild West”, and the opportunity to make a killing. And he literally did. Marketing a dilute solution of sulfuric acid colored with red wine, his “Microbe Killer”, widely advertised and sold often in religious/theatrical “fire and brimstone” revival sessions (promising to “Cure All Diseases” – a phrase embossed on its glass bottle), he made a quick fortune. Taken in high doses, it also killed a few people.
Retail Pharmacy: The Nucleus of the Pharmaceutical Industry. Part I – The Local Druggist
Posted on | September 5, 2019 | 3 Comments

Mike Magee
If you do a word association game today, and throw out the word “sickness”, many will respond with “medicine”. If you query “medicine, “drug store” or “pharmacy” appear. Press further, and CVS and Walgreens make the list. This is not a phenomena of health consumerism which as a movement is scarcely three decades old. No, it has a rich tradition, one that is as old as our nation itself.
Americans have always loved their medicines and sought them out actively to cure whatever ailed them. Their interest ranged all the way from “staying well” to “feeling better.” Productivity in this hard-charging, “pull yourself up by the bootstraps” society required activity, and it’s hard to be active when you’re sick.
As a doctor’s family in the 1950’s, we were a medicine family. If you, as a 10 year old, had an upset stomach or diarrhea, you went to our refrigerator, and inside you would reliably find a one quart brown bottle of paregoric cremosuxidine, an opium laced remedy. Take a swig right out of the bottle and you immediately felt better.
The medicine came from Mr. Julius Jones who ran the drug store and soda fountain across the street from our house. When my father received his M.D. in 1942, there were 80,000 pharmacists in the U.S., but only 3000 worked at hospitals. Most were small retail operations built around the practice of compounding medicines. Elixirs, suspensions, ointments, creams, capsules, powders and suppositories constituted an ever changing product line. By 1942, guidance for the druggist came from one reliable source – United States Pharmacopeia (USP) guide – 11th Edition (1937) or 12th edition (1943). This text not only catalogued approved medicines but also the various formulations or recipes for their execution and delivery from behind the counter. Even at this time however, pharmacy was becoming standardized. Fully 70% of prescriptions could be filled with pre-packaged medications.
Mr. Jones was the product of an accelerated 3-year training program instituted in the build up to World War II. Before that, and ever since 1932, a four year Bachelor of Science degree in pharmacy was mandatory. By 1942, there were sixty-eight colleges of pharmacy in the U.S. The training programs focused on the science, techniques and business of medicines. State licenses were not reciprocal across state borders.
My father’s office, on the corner of Columbia Avenue and Abbott Boulevard, two blocks from the Palisades Amusement Park and the Palisade Cliffs, was attached to our house. Mr. Jones’ store was as much a fixture on the “Junction” as was Kate and John’s Delicatessen. The block long collection of some ten or so one-story local businesses had been on the trolley line connecting Hudson County towns like West New York and Jersey City to Fort Lee. The trolley that stopped at this junction no longer ran. But the name “junction” stuck.
In any case, this was the meeting point, where people from Cliffside Park, and Edgewater, and Fort Lee would congregate to see my father when they were ill. No appointments were required. It was a walk-up, and largely a cash business. The poor were seen, relying on my father’s benevolence and good will, which was substantial.
My father likely was able to maintain his good humor in part because of his personal and professional friendship with the druggist, Julius Jones, who was considerably more rigid when it came to payment. In fact, it was Mr. Jones who instructed me one day, on seeing me pick up a penny someone had left on the store floor, to “never throw away a penny. Ten of them will make a dime; and ten of those a dollar. That’s how I got rich – I never threw away a penny.”
In fact, Mr. Jones mainly got rich through associations and relationships with local doctors. And my father, being very active and just across the street, was customer #1. The store’s revenue stream was split between sales from behind the counter, at the counter, and in front of the counter. In front, there were a wide variety of household durable goods. The shelves were meticulously stacked with proprietary medicines, toiletries, hair curlers and pins, makeup, stockings, and of course candy and cigarettes. At the counter was a full-on soda bar (including sundaes in thick ice cream glasses and black and white (chocolate soda and vanilla ice cream) ice cream sodas with 5 green vinyl covered circular twister seats. And behind the counter, off to the side, were large bottles filled with pills and tablets, lotions and potions, and solid granules of varying colors, sizes and textures, and a worn, stone mortar and pestle. Concoctions were mixed to order, following complex prescriptive directions, written in Latin – the preferred language between doctor and druggist, which effectively kept the patient out of the loop.
Growing up in the 1950’s, I was largely unaware that this quaint retail outlet, and thousands of others like it, was in fact the birth place of the pharmaceutical industry. But that was truly the case. In fact, one seminal published paper at the turn of the century was correctly titled, “Retail Pharmacy as the Nucleus of the Pharmaceutical Industry”. That paper recounted that in the 17th century in Europe, primitive medicinal chemists, running stores the size of Mr. Jones’s, were busy in the back room producing a range of products for wholesale distribution close and far away.
Part II: The European Apothecary (next)
What We Don’t Know.
Posted on | August 27, 2019 | Comments Off on What We Don’t Know.
Mike Magee
Some years back, I asked Craig Ventor, co-discoverer of the human genome, what percentage of the knowledge he believed we currently possessed to take optimal care of human beings. His rapid response? “Less than 1 percent.”
Austin Frakt, public health professor at Boston University and Harvard’s T.H. Chan School of Public Health, recently highlighted lack of evidence in equally dramatic terms. He cited a British Medical Journal analysis that confirmed that evidence of benefit does not exist for over 50% of current medical treatments.
Frakt says the problem extends into the health policy arena as well, a theme I drum repeatedly in CODE BLUE: Inside the Medical Industrial Complex. His words: “Much of what we do lacks evidence; and even when evidence mounts that a policy is ineffective, our political system often caters to invested stakeholders who benefit from it.”
The absence of evidence is nothing new in America’s history, a fact that has been made abundantly clear in my preparation for a Fall offering at the President’s College at the University of Hartford titled, “The President’s Hidden Health Record – From FDR to Trump – and How It Shaped America.”
Beginning with George Washington, whose death was hastened by a toxic mixture of induced bleeding and enforced purgatives, our Presidents (and the citizens who elected them) have been poorly served by the medical establishment of their days.
Adding to the confusion, Presidents and their White House doctors have routinely conspired to hide serious and at times life threatening medical conditions in an effort to be elected and stay in office. They have taken mind-altering drugs with abandon. They have altered or destroyed medical records. They have continued to hold tightly onto the reins of power while mentally or physically unfit.
Even with full disclosure, as Frakt outlines, “It is not uncommon for newer evidence to contradict what had been standard practice. A study by an Oregon Health & Science University School of Medicine physician, Vinay Prasad, and colleagues examined 363 articles in the New England Journal of Medicine from 2001 to 2010 that addressed an existing medical practice. Forty percent of the articles found the existing practice to be ineffective or harmful.”
States like North Carolina are wading into performance payment systems, promising insurers that, in the future, they will “pay for health not health care.” But to deliver on that promise will require quite an investment in medical humility, including: research transparency, full disclosures, real-time evaluation and application of evidence, and knowledge transfer to health professionals, patients, families and communities.
In that pursuit, knowing what we don’t know will prove to be at least as important as knowing what we do know.
AMA’s Quiet Retreat
Posted on | August 20, 2019 | 2 Comments

Mike Magee
It’s the dog days of summer. So you may have missed a brief, but significant announcement by the AMA last week that it was exiting the anti-“Medicare-for-all” coalition, The Partnership for America’s Health Care Future. It is a faux-partnership whose real purpose is to preserve the past rather then chart a progressive future.
The party line, voiced by the CEO of the for-profit hospital association (a member), is “We have a structure that frankly works for most Americans. Let’s make it work for all Americans. We reject the notion that we need to turn the whole apple cart over and start all over again.”
So why is the AMA leaving? The party line voiced by AMA president James Madara was “The AMA decided to leave the Partnership for America’s Health Care Future so that we can devote more time to advocating for these policies that will address current coverage gaps and dysfunction in our healthcare system.” The truth is the organization was increasingly uncomfortable with tactics, messaging and the company they were keeping. As one anonymous insider said, “we need to move on and not only talk about what we’re against but what we’re for.”
The AMA found itself on a slippery slope with members that packed a wallop. Its 27 member lobbying effort has been intentionally on the “down-low”; a quasi-organization that actively hid its parentage.
In the interest of transparency, here’s a list of the original Leaders and Followers .
Leaders:
1. American Medical Association (AMA) – the doctors
2. American Hospital Association (AHA) – the non-profit hospitals
3. Federation of American Hospitals (FAH) – the for-profit hospitals
3. America’s Health Insurance Plans (AHIP) – the major insurers
4. Pharmaceutical Research and Manufacturing Association (PhRMA) – the drug makers
5. Biotechnology Innovation Organization (Bio) – the biotechnology companies
6. Association for Accessible Medicines (aam) – the generic drug producers
7. Council of Insurance Agents and Brokers (The Council) – the health insurance brokers
8. Healthcare Leadership Council (HLC) – the coalition of MIC CEO’s
9. National Association of Insurance and Financial Advisers (NAIFA) -The financial/insurance industry
10. National Association of Health Underwriters (NAHU)
Followers:
2. Hospital Corporation of America (HCA)
3. Ascension Health (largest Catholic HC System)
5. Community Health Systems (CHS)
6. Life Point Health (Holding Company for 70 health care institutions)
7. Tenet Health
8. UHS (Universal Health Services) – manages 350 hospitals
9. Texas Health Resources (faith based 29 hospital system)
10. Premier Inc. (Health Data mining company)
11. Life Point Health (Holding Company for 70 health care institutions)
13. North Dakota Medical Association (NDMA)
14. American College of Radiology
What can we take away from the AMA retreat. Hcom sees it as a signal that three realities are coalescing:
- Public support for universal health coverage is overwhelming and here to stay.
- Waste and inefficiency resulting from the excesses of the Medical-Industrial Complex are increasingly in the cross-hairs, and potentially compromise physicians future economic prospects. (There are 16 health care workers now for every one physician.)
- If the battle to be waged against the status quo is between the MIC and patients, it appears the AMA is positioning itself to line up with the patients.


